Abstract
Primary myeofibrosis (PMF) is one of the Ph negative myeloproliferative neoplasms (MPN). The mainly clinical features are obviously physical symptoms and symptomatic splenomegaly. It may be converse to leukemia and has shortened life expectancy. Nowadays, the therapy of PMF is aimed at maintaining comfort and there was no effective treatments. PMF complicated with myelodysplastic syndrome (MDS), which is named as MDS/MPN-u, is a rare case, and the treatments are confused. In this study, we want to discuss an effective treatment in MDS/MPN via a case therapy and literature review.
A 55-year-old woman presented with fatigue and chest distress for one month was admitted in our hospital. Physical examinations showed anemic appearance and splenomegaly which was four fingers under lib. A routine blood count test showed pancytopenia. A bone marrow examination showed dysplasia and fibrous tissue proliferation. The JAK2/V617F mutation was positive and the expression was 60.63%. The chromosome karyotype showed 47, XX, t (1; 20) (p11.2; q11.2), +9,-13, +21. She was diagnosed as PMF complicated with MDS (MDS/MPN) according to WHO 2016 version of hematologic neoplasms classification. She received thalidomide 100mg daily therapy combined with prednisone.
10 months later, The patient presented obviously physical symptoms and progressive splenomegaly, accompanied with higher blasts. These manifestation reflected that the disease was progressed and the previous treatment was failure which was thalidomide and prednisone. Then, she received new therapeutic method with low-dose DAC. She was administered DAC at 15mg/m2 weekly via intravenous infusion over one hour. Three times a cycle and every 4 weeks a course. If the disease was improved, the dosing interval would be extended.
Results
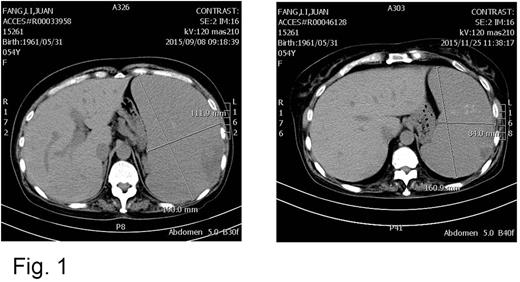
After two cycles, the bone marrow smear showed the blasts was decreased to 0.5%, and abdominal CT showed the spleen was shrank (Fig.1). After four cycles, she felt comfortable and the peripheral blood count was improved towards normal. The treatment interval was prolonged. After 8 cycles, the spleen reduced to 2cm under rib, and hematological remission was achieved. After 10 cycles, the mutation of JAK2/V617F expression was decreased from 60.63% to 0.01%. During the therapy, the patient presented grade III-IV hematological toxicity at first two cycles, and there were no side effect happened at following cycles.
Discussion
PMF patients face a series of clinical problems, such as anemia, spleen enlargement, physical symptoms, and symptomatic medullary hematopoiesis.1-3 We should recognize to deal with these problems as early as possible and give appropriate treatment. Thalidomide combined with prednisone was used for MF patients with moderate to severe anemia, and it was one of the first-line treatment of MF at present.
The recently studies had demonstrated gene inactivation of tumor-suppressors due to abnormal DNA methylation part contributes the pathogenesis of MF and MDS/MPN.4 5-Aza-2′-deoxycytidine (decitabine, DAC) has been suggested to exert antineoplastic effects through the inhibition of DNA methyltransferases (DNMT), causing DNA hypomethylation, and it was widely used in MDS and AML nowadays. DAC was also used in a clinical trial in 21 patients of MF and achieved clinical response.5
This patient was diagnosed as PMF complicated with MDS, and she was given thalidomide and prednisone for the first line therapy. However, after 10 months therapy with thalidomide and prednisone, the disease was progressed. It was appeared with obviously physical symptoms, progressive splenomegaly, and gradually pancytopenia. Then, she received low-dose DAC as second line therapy and achieved hematological remission. Our research indicated that low-dose DAC was an effective and safe treatment in MDS/MPN, especially in improving physical symptoms and pancytopenia.
Funding: Social development project of public welfare technology research, Zhejiang Provincial Department of science and technology, Zhejiang Province, China (2016C33160). Public technology research projects of Yiwu City, Zhejiang Province, China (2016-S-05).
Correspondending author information: Dr. Jian Huang, Department of Hematology, The fourth Affiliated Hospital, College of Medicine, Zhejiang University. No. N1 Shangchengdadao Road, Yiwu 322000, Zhejiang Province, People's Republic of China. Email: househuang@zju.edu.cn
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal